Mohs surgery is a highly effective treatment method for certain types of skin cancer. This specialized procedure is designed to remove cancerous skin cells while preserving as much healthy tissue as possible. Mohs surgery offers several advantages over traditional excisional surgery, including a lower risk of recurrence and improved cosmetic outcomes. In this blog post, we will explore the various types of skin cancers that are treated with Mohs surgery, shedding light on the specifics of each cancer type and the rationale for choosing this surgical technique. Texas Surgical Dermatology, led by Dr. Tri H. Nguyen who is a Mohs fellowship-trained specialist, provides treatment of skin cancer to patients in Houston, Katy, Spring, The Woodlands, Texas, and surrounding locations.
Mohs surgery is a highly effective treatment method for certain types of skin cancer. This specialized procedure is designed to remove cancerous skin cells while preserving as much healthy tissue as possible. Mohs surgery offers several advantages over traditional excisional surgery, including a lower risk of recurrence and improved cosmetic outcomes. In this blog post, we will explore the various types of skin cancers that are treated with Mohs surgery, shedding light on the specifics of each cancer type and the rationale for choosing this surgical technique. Texas Surgical Dermatology, led by Dr. Tri H. Nguyen who is a Mohs fellowship-trained specialist, provides treatment of skin cancer to patients in Houston, Katy, Spring, The Woodlands, Texas, and surrounding locations.
Introduction to Mohs Surgery and Its Benefits
Mohs micrographic surgery is a specialized procedure developed in the 1930s by Dr. Frederick Mohs. This method involves the meticulous removal of cancerous skin layers, which are then examined microscopically for the presence of cancer cells. If cancerous cells are identified, additional layers are excised until no cancer remains. This systematic approach allows for highly targeted treatment, making it particularly effective for certain skin cancers.
One of the key advantages of Mohs surgery is its impressive cure rate, which can reach up to 99% for specific types of skin cancers like basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). This high success rate is partly due to the detailed examination of excised tissues during the procedure, ensuring complete cancer removal.
Another significant benefit is the preservation of healthy tissue. Traditional excisional surgeries often remove a larger margin of skin to ensure all cancerous cells are eliminated, which can lead to more significant scarring and tissue loss. In contrast, Mohs surgery removes only the affected tissue, sparing as much healthy skin as possible. This is particularly advantageous for cancers located in cosmetically sensitive areas such as the face, neck, and ears, where minimizing visible scarring is essential.
Additionally, Mohs surgery offers immediate results, as the tissue is examined on-site during the procedure. If any cancer cells are detected in the examined layers, they can be promptly removed, reducing the likelihood of needing multiple surgeries. This real-time assessment ensures that patients leave the surgical appointment knowing their cancer has been thoroughly treated.
For these reasons, Mohs surgery is often recommended for skin cancers that are recurrent, located in high-risk or cosmetically sensitive areas, or have aggressive growth patterns. Its combination of high cure rates, tissue preservation, and immediate results makes it a highly effective treatment option for various types of skin cancers.
Basal Cell Carcinoma: The Most Common Skin Cancer
Basal cell carcinoma (BCC) is the most prevalent type of skin cancer, making up about 80% of all diagnosed cases. BCC usually develops due to prolonged exposure to ultraviolet (UV) radiation, typically from the sun. It often manifests as a pearly bump or a flat, brownish scar-like lesion, most commonly appearing on sun-exposed areas of the skin such as the face, neck, and arms.
Mohs surgery is often the preferred treatment for BCC for several compelling reasons:
- **Aggressive Growth:** BCC can be locally aggressive, invading surrounding tissues if not treated. Mohs surgery ensures precise and complete removal of cancerous cells, which is critical for preventing further tissue invasion.
- **High Recurrence Rate:** Although BCC is generally not life-threatening, it has a notable tendency to recur, especially in individuals with a history of skin cancer. The precision of Mohs surgery minimizes the risk of recurrence by targeting and removing all cancerous cells.
- **Cosmetic Considerations:** BCC frequently occurs in cosmetically sensitive areas like the face and neck. Mohs surgery’s tissue-sparing technique helps preserve as much healthy skin as possible, leading to better cosmetic outcomes compared to traditional surgical methods.
Given these factors, Mohs surgery is often recommended for patients with BCC, especially those with lesions in areas where preserving appearance is crucial. The combination of high cure rates, reduced recurrence, and minimal scarring makes Mohs surgery an optimal choice for treating basal cell carcinoma.
Squamous Cell Carcinoma: A Commonly Treated Cancer with Mohs Surgery
Squamous cell carcinoma (SCC) is a prevalent skin cancer that exhibits a more aggressive behavior compared to basal cell carcinoma (BCC). Typically arising in sun-exposed areas such as the face, ears, neck, and hands, SCC can present as a firm, red nodule, a scaly patch, or an ulcerative lesion that does not heal.
Mohs surgery is particularly beneficial for treating SCC due to its meticulous layer-by-layer removal technique. This method ensures comprehensive excision of cancerous cells while preserving surrounding healthy tissue. The precise nature of Mohs surgery is critical for SCC because this type of cancer has a higher propensity to invade deeper skin layers and, in some cases, metastasize to other parts of the body if left untreated.
For patients with a high risk of recurrence, such as those with multiple SCC lesions or compromised immune systems, Mohs surgery provides a targeted approach that significantly reduces the likelihood of the cancer returning. The on-site microscopic examination of excised tissues ensures that all cancerous cells are removed during the initial procedure, minimizing the need for additional surgeries.
Additionally, SCC often develops in cosmetically and functionally sensitive areas, making the tissue-sparing aspect of Mohs surgery particularly valuable. This surgical technique aims to remove only the cancerous tissue, leading to better cosmetic and functional outcomes for patients. Immediate microscopic examination during the surgery further ensures that patients receive a thorough and effective treatment in one session, reducing the overall treatment time and associated stress.
In summary, Mohs surgery’s precise, tissue-conserving approach makes it an excellent option for managing squamous cell carcinoma, particularly in high-risk cases and sensitive anatomical locations.
Treating Melanoma In Situ with Mohs Surgery
Melanoma in situ represents the earliest stage of melanoma, confined to the top layer of the skin. At this stage, the cancer has not yet invaded deeper tissues or spread to other parts of the body, making early and effective treatment crucial. Mohs surgery offers several significant benefits for addressing melanoma in situ.
One of the primary advantages of using Mohs surgery for melanoma in situ is its unparalleled precision. This technique allows for the meticulous removal of cancerous cells, layer by layer, which is particularly important for melanoma due to its potential for irregular and diffuse borders. Each excised layer is examined microscopically in real-time, ensuring that all cancerous cells are identified and removed during the procedure. This thorough examination helps to confirm clear margins and reduces the risk of the melanoma progressing or recurring.
The preservation of healthy tissue is another critical benefit of Mohs surgery, especially for melanoma in situ. By removing only the affected layers of skin, Mohs surgery minimizes tissue loss and scarring, which is particularly beneficial for lesions located in highly visible or cosmetically sensitive areas such as the face. This approach not only addresses the cancer effectively but also prioritizes the patient’s aesthetic and functional outcomes.
Additionally, the ability to achieve immediate results is invaluable in treating melanoma in situ. Patients undergoing Mohs surgery receive instant feedback on whether all cancerous cells have been removed, eliminating the uncertainty and waiting period typically associated with traditional surgical methods. This real-time assessment ensures comprehensive treatment in a single surgical session, providing peace of mind and reducing the overall treatment burden.
Although Mohs surgery is more commonly associated with non-melanoma skin cancers like basal cell carcinoma and squamous cell carcinoma, its application in melanoma in situ is growing due to these distinct advantages. The technique’s precision, real-time assessment, and tissue preservation make it a highly effective treatment option for early-stage melanoma, offering patients the best chance for a positive outcome with minimal cosmetic impact.
Uncommon Skin Cancers: When Mohs Surgery is Still an Option
Mohs surgery is not only effective for common skin cancers but also holds promise for treating several uncommon types. These less prevalent cancers often require specialized treatment approaches due to their unique characteristics and potential for aggressive behavior.
**Merkel Cell Carcinoma:** This rare but aggressive skin cancer demands precise and thorough treatment to prevent metastasis. Mohs surgery excels in this area by meticulously removing cancerous cells layer by layer, ensuring no malignant cells are left behind. This detailed approach significantly reduces the risk of recurrence and helps in managing this high-risk cancer effectively.
**Dermatofibrosarcoma Protuberans (DFSP):** DFSP is a rare, slow-growing tumor that often recurs if not entirely excised. Mohs surgery offers a high level of precision in removing this type of cancer, minimizing the chance of recurrence. The method’s ability to confirm clear margins through microscopic examination during the procedure is crucial for long-term patient outcomes.
**Lymphomas:** Certain types of skin lymphomas, which can manifest as localized lesions, are also treatable with Mohs surgery. This technique is beneficial for ensuring complete removal while conserving as much healthy tissue as possible, an essential factor in reducing the impact of surgery on the patient’s quality of life.
By applying the precise and tissue-sparing techniques of Mohs surgery, healthcare providers can effectively treat these uncommon but challenging skin cancers. This approach not only improves the chances of complete cancer removal but also enhances cosmetic and functional outcomes for patients, making it a valuable option for managing various rare skin malignancies.
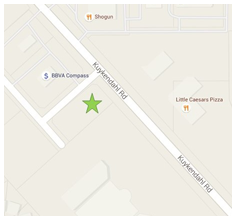
For More Information contact our Board Certified in Dermatologists at Texas Surgical Dermatology in Spring, TX
For more information on procedures and treatments offered at Texas Surgical Dermatology PA please call 832.663.6566 or click here to contact our dermatologists. Helping patients in Houston, The Woodlands, Spring, Katy and other surrounding areas of Texas.